Achalasia is an uncommon condition of the oesophagus where the valve (known as the lower oesophageal sphincter), at the lower end of the oesophagus doesn’t open to allow food through when you swallow. As well as the valve not opening properly, the oesophagus stops contracting properly and pushing food down into your stomach. Longer term this can cause your oesophagus to dilate and become distended.
People suffering from achalasia always have trouble swallowing, often have chest pain, regurgitation symptoms and can be losing or having trouble maintaining weight. Often you will have been treated unsuccessfully for reflux for some years before your diagnosis.
How is it diagnosed
Although your doctor may be suspicious based on your history and results from gastroscopy or barium meal (xray test), patients with achalasia all need referral for a pH/manometry test. This is a test where a thin wire is placed into through your nose, into your gullet/oesophagus, and the pressure in your oesophagus is measured whilst you drink sips of water. Currently this is not available on the coast, and required referral to Newcastle or Sydney. Dr Hamer or your gastroenterologist will arrange this referral for you.

Operation – key hole surgery – laparoscopic cardiomyotomy
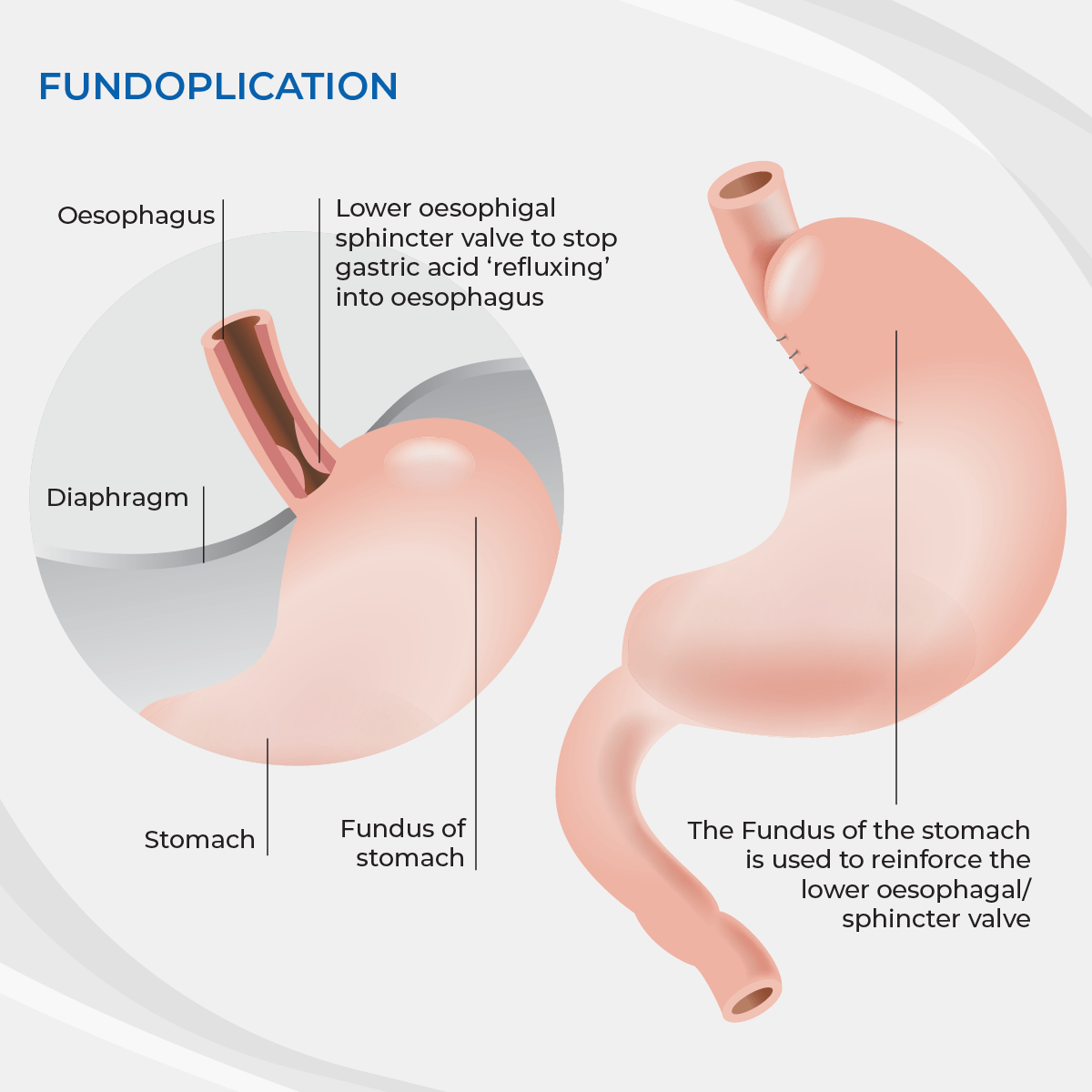
Achalasia can be effectively treated by a key hole operation cause laparoscopic cardiomyotomy. This is an operation to divide the muscle of the lower oesophageal sphincter (the valve that won’t open), to allow food through when you swallow. After opening the valve up, swallowing improves, but stomach acid can also reflux back into the oesophagus. To prevent this, a partial fundoplication (an anti-reflux operation) is performed at the same time. This returns the valve to as close as normal as possible – allowing food through, but also stopping reflux. After cardiomyotomy your oesophagus may start to contract (peristalsis) to some degree again, but unfortunately it is rare for it to return to normal completely. This is true with all treatments for achalasia.
Laparoscopic cardiomyotomy is done as key hole surgery, requiring in most cases an overnight stay in hospital. Patients feel an immediate improvement in their swallowing.
Other treatments
POEM (per oral endoscopic myotomy) is an endoscopic method to divide the lower oesophageal sphincter. Although it divides the valve well, it leaves approximately 50% of people with reflux and needing to be on lifelong anti-reflux tablets. People also need to spend on average an extra day in hospital compared with laparoscopic cardiomyotomy.
Pneumatic dilatation
Using an endoscope, a pneumatic balloon is used to stretch the sphincter (valve) to weaken it to allow food through. Although this can be effective in a lot of patients, multiple dilatations can be needed to achieve a good result. If the oesophagus is perforated during the procedure (1/20 risk), you will need an emergency operation to repair the perforation.
Botox
Botox can be injected into the sphincter to relax it. Unfortunately this wears off after 3-6 months.
Side effects to be aware of
All operations have side effects or potential complications you need to be aware of. Risks of any operation include the risk of the anaesthetic, small risks of bleeding, infection and hernias developing in the key hole entry sites. Specific to laparoscopic cardiomyotomy you need to know that your surgeon is operating in the area of major blood vessels called the aorta and the vena cava, nerves which help the stomach to empty, the oesophagus, stomach, liver and spleen. Although injuries to these are rare, they can occur.
Although the lower oesophageal sphincter can be divided allowing food to pass, the oesophagus may not regain its normal function, and although your symptoms will improve dramatically, you should not expect your swallowing to return completely to normal. In about 10% of people the oesophagus will continue to worsen despite having had correct treatment.
What to expect
For 3 days before the operation you should be on a ‘free fluid’ diet only. This allows the oesophagus to empty before your operation.
You will be admitted to the hospital on the day of your operation. You will meet the nursing staff and the anaesthetist who will be administering your anaesthetic. After your operation you will wake up in the recovery area of the hospital where specialized recovery nurses will look after you and ensure you recover from your anaesthetic safely. After this you will be moved either to the ward. At any stage if the nurses have concerns about your recovery they will contact your anaesthetist or Dr Hamer. After waking up from your operation you will initially be allowed water to drink. After this you will be allowed to try some food of a pureed consistency.
After your operation
Diet:
You will need to be careful with what you eat after your cardio-myotomy. For the first month you should eat only very soft foods that don’t require a lot of chewing. You should avoid bread, red meat and pasta. You should avoid fizzy drinks during this period. After a month you can slowly start trialing a normal healthy diet again. If you are having trouble with any particular food simply stop and try again in a week or two.
After you have been discharged from the hospital, you will have dressings over your wounds. These do not affect how well your wounds heal, but they do protect your clothes from any seepage which may occur. If they become dirty or wet they may simply be removed and changed for a similar dressing or a band aid. After a week they can be removed and discarded. Occasionally people feel more comfortable leaving a dressing on for an extra week, particularly if the wound is somewhere that can rubs on your clothing.
Sutures:
Your wounds will be closed with either glue or dissolving sutures, neither of these need removal.
Pain killers:
Most people find taking regular paracetamol to be enough for their pain. Paracetamol has the advantage (unlike most other pain killers) that it won’t make you constipated or feel woozy. It is also very safe if taken carefully according to the instructions on the packet. In some circumstances you will be given additional pain killers to take home with you. If this is the case, you should read and follow the instructions carefully.
Problems:
Complications are unusual. If you do have any problems you have multiple ways of accessing help. During office hours you can contact Dr Hamer’s rooms or your GP. For more pressing problems or after hours you can also contact the emergency department at the hospital.
Recovery:
Generally most people find that they are fit to return to light duties at work after 1 -2 weeks. You should avoid heavy lifting for four weeks after your operation. If you are still having significant problems at this time you should be reviewed to ensure you are still recovering properly.
Follow Up
You will be reviewed 4-6 weeks after your operation to ensure you have recovered. Dr Hamer will discuss the need to do an endoscopy to look for any precancerous changes that can occur.
